Human trial data published in a major journal show that statins cause insulin resistance and deplete GLP-1 levels in humans. This should have been breaking news! Why is no one talking about it? Why don’t doctors know? Why aren’t patients being informed about the risks?
For references and a written breakdown, see the StayCurious Metabolism Newsletter: open.substack.com/pub/staycuriousmetabolism/p/this-study-should-have-changed-medicineno
Summary Provided By AI LLM NoteGPT.io
Summary
The video transcript discusses a significant yet underreported scientific study on statins, the world’s most profitable drug class, and their adverse effects on insulin resistance, type 2 diabetes risk, and especially GLP-1 levels in humans. While it is somewhat known that statins may increase diabetes risk, the study reveals a substantial and direct reduction of GLP-1—a hormone critical in glucose metabolism and the target of popular diabetes and weight loss drugs known as GLP-1 receptor agonists. This creates a paradox where a widely prescribed medication (statins) may worsen the biological pathway targeted by cutting-edge therapies. The research, published in Cell Metabolism in early 2024 but largely ignored in medical circles and media, involved human trials, mouse models, and microbiome analyses. It demonstrated that statins disrupt gut microbiota, specifically depleting Clostridium species responsible for converting bile acids into ursodeoxycholic acid (UDCA), a compound that supports GLP-1 production and insulin sensitivity. Supplementing with UDCA reversed the negative metabolic effects of statins in both mice and a small human pilot study.
The speaker expresses frustration that these findings have not permeated clinical practice or medical education and critiques the healthcare system’s profit-driven incentives that hinder the adoption of simple, inexpensive, and effective adjunct therapies like UDCA supplementation. The video ends with a call to action for patients and clinicians to become aware of these findings, foster dialogue, and advocate for improved care that prioritizes patient well-being over pharmaceutical profits.
Highlights
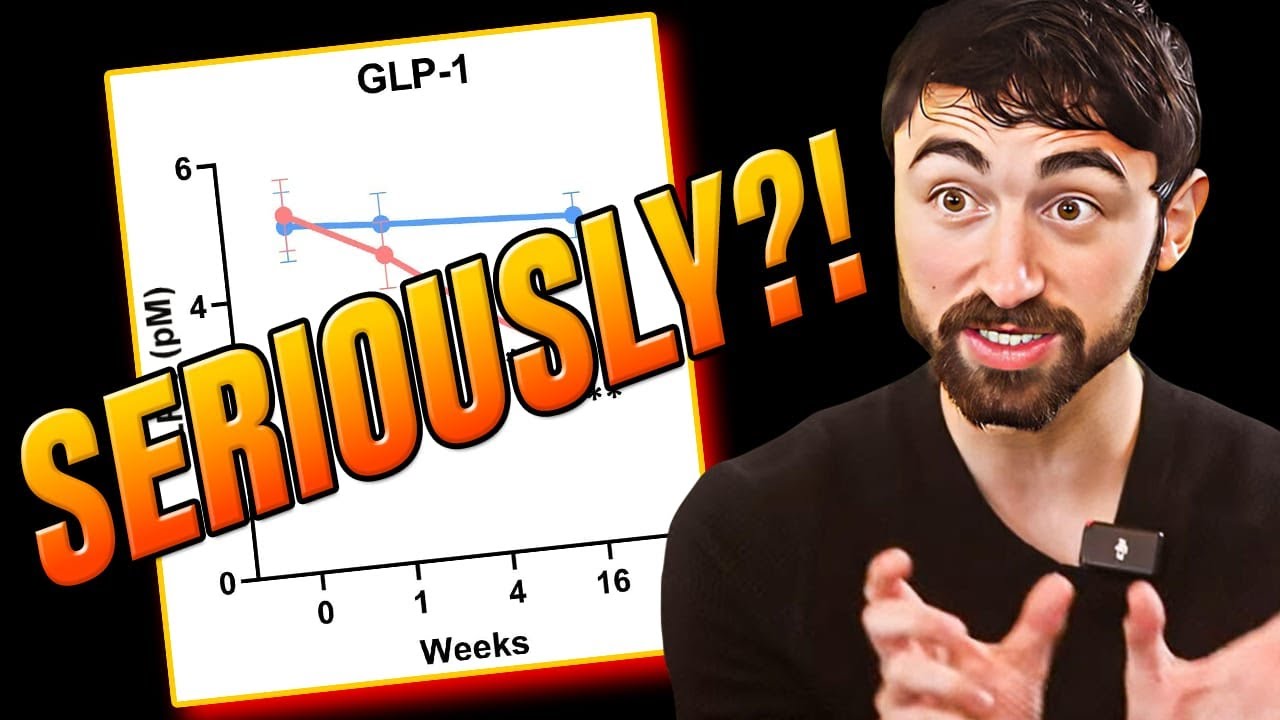
- 💊 Statins, prescribed to 1 in 4 people over 40, significantly reduce GLP-1 levels by nearly 50%.
- 🧬 Statins disrupt gut microbiome by depleting Clostridium bacteria, leading to lower production of beneficial bile acid UDCA.
- 🐭 Mouse studies confirmed that statin-induced microbiome changes cause insulin resistance and reduced GLP-1, which can be reversed by UDCA supplementation.
- 🧪 A small human pilot trial showed that UDCA supplementation improved blood sugar, insulin resistance, and restored GLP-1 levels in statin users.
- 📉 Despite strong, peer-reviewed evidence published in Cell Metabolism, these findings remain obscure in medical education and clinical practice.
- 💡 The healthcare system’s profit-driven incentives often suppress simple, effective adjunct treatments that are inexpensive and biologically sound.
- 🔍 The video encourages patients and clinicians to share this information, question current practices, and prioritize patient-centered care.
Key Insights
-
🔬 Statins and GLP-1: A Hidden Metabolic Disruption
The study reveals a novel and critical metabolic side effect of statins: a near 50% reduction in GLP-1 levels. GLP-1 is essential for stimulating insulin secretion and regulating blood glucose. This insight is particularly important given the simultaneous rise in GLP-1-based therapies for diabetes and obesity. The fact that statins undermine GLP-1 levels suggests a complex, counterproductive interaction between widely prescribed cholesterol-lowering drugs and modern metabolic treatments, which has been largely overlooked. -
🦠 Gut Microbiome as the Mediator of Statins’ Side Effects
The research identifies how statins alter the gut microbiome, specifically depleting Clostridium species that convert primary bile acids into UDCA, a secondary bile acid crucial for maintaining insulin sensitivity and GLP-1 secretion. This mechanistic link between gut bacteria, bile acid metabolism, and systemic glucose homeostasis highlights the importance of microbiome health in drug side effects and metabolic diseases. -
🐁 Animal Models Confirm Causality and Reversibility
Mouse experiments were pivotal in confirming that microbiome changes caused by statins directly lead to insulin resistance and GLP-1 reduction. Furthermore, reintroducing Clostridium or supplementing with UDCA reversed these effects, demonstrating that the metabolic damage is not permanent but modifiable. This reversibility opens the door for therapeutic interventions that could mitigate statin-induced diabetes risk. -
👨⚕️ Lack of Awareness Among Physicians Reflects Systemic Gaps
An informal poll of physicians, including cardiologists, revealed widespread ignorance or uncertainty about statins’ effects on GLP-1. This knowledge gap underlines systemic issues in medical education and continuing professional development, where emerging but clinically relevant findings fail to reach frontline clinicians. It also underscores the challenge patients face in receiving fully informed care. -
💸 Profit Motive as a Barrier to Optimal Patient Care
The speaker argues that financial incentives within healthcare prioritize drug sales and protocol adherence over patient-centered approaches that might include inexpensive supplements like UDCA. This misalignment results in inertia and silence around simple, safe, and effective solutions that could improve patients’ metabolic outcomes without additional costly medications. -
💊 UDCA Supplementation as a Promising Adjunct Therapy
UDCA, available as a supplement and shown to restore GLP-1 levels and improve glucose metabolism in both animal models and a small human pilot, represents a low-cost, low-risk intervention. Its potential to counteract statin-induced metabolic harm is significant, especially given the prevalence of statin use worldwide. However, clinical guidelines have yet to incorporate this option, reflecting a gap between research and practice. -
📢 The Call for Patient and Clinician Empowerment
The video ends with an urgent appeal for awareness, transparency, and dialogue. Patients should be informed and encouraged to discuss these findings with their healthcare providers. Clinicians and medical students should critically evaluate current practices, incorporate emerging evidence, and advocate for systems that prioritize holistic health over profits. This empowerment is essential for improving outcomes and restoring trust in medicine.
Conclusion
This video transcript conveys a compelling narrative that highlights an important but neglected side effect of statins—significant suppression of GLP-1 via microbiome disruption and bile acid metabolism alteration. The findings are robust, translational, and clinically meaningful, yet remain underrecognized in medical and public domains due to systemic inertia and profit-driven healthcare structures. The demonstrated benefit of UDCA supplementation offers a practical, evidence-supported strategy to mitigate adverse metabolic effects of statins. Ultimately, the video serves as both an educational resource and a call to action, urging healthcare stakeholders to bridge gaps between research, clinical practice, and patient empowerment for better metabolic health outcomes.

Here is the paper:
https://doi.org/10.1016/j.cmet.2023.12.027 - Statins aggravate insulin resistance through reduced blood glucagon-like peptide-1 levels in a microbiota-dependent manner
Probably should do a full read of the paper soon